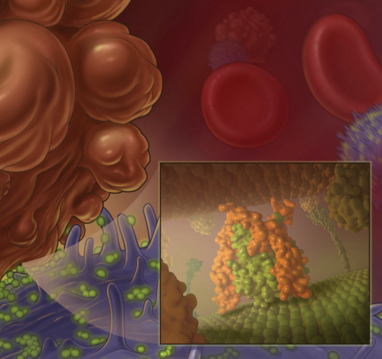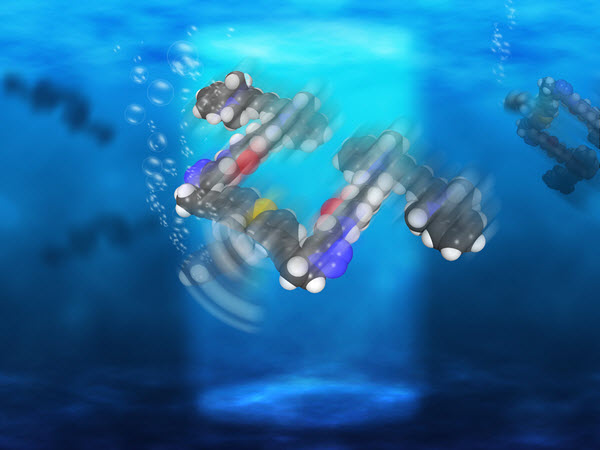
Rice University scientists have created light-driven, single-molecule submersibles that contain just 244 atoms (credit: Loïc Samuel/Rice University)
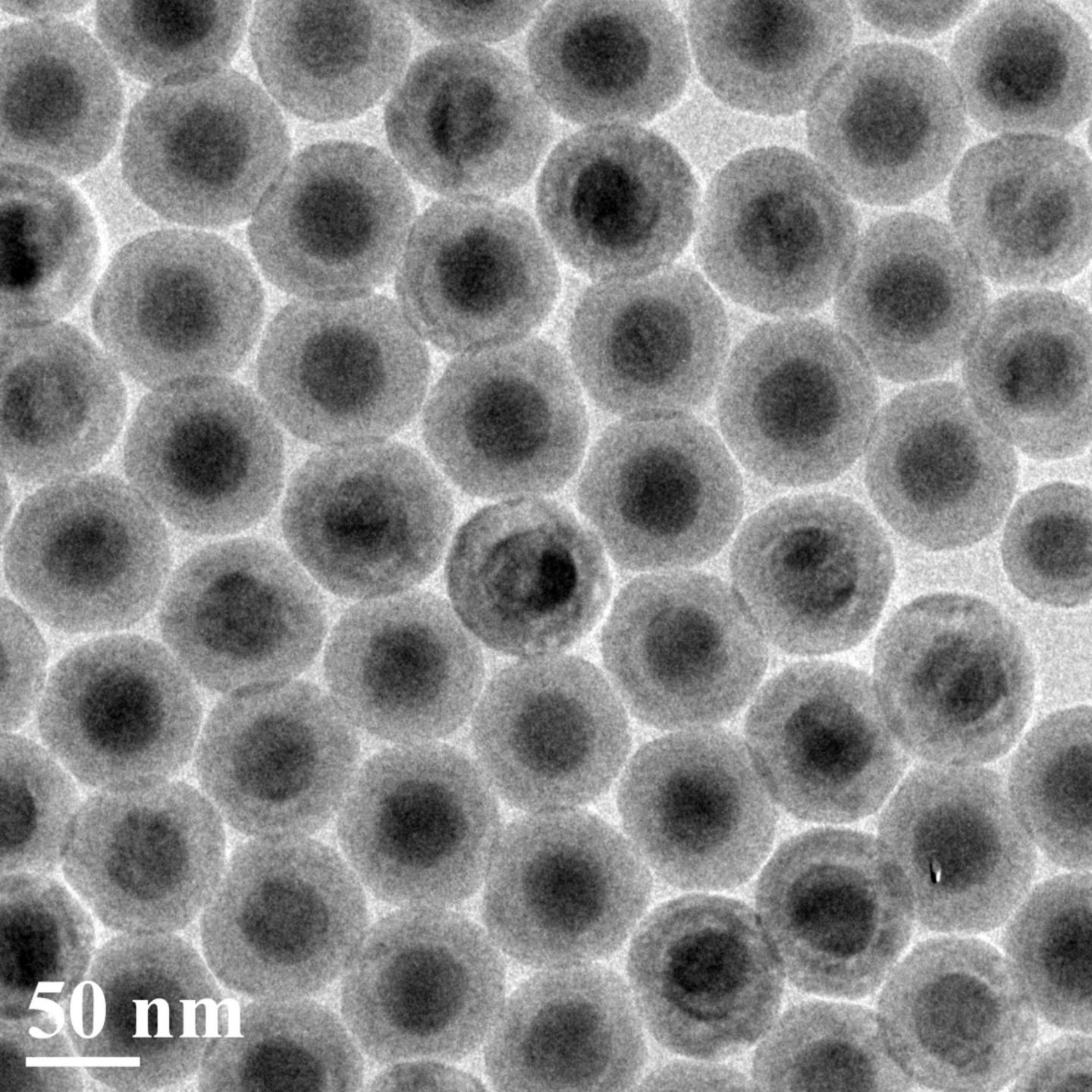
The Rice University lab of chemist James Tour has created single-molecule, 244-atom submersibles with motors powered by ultraviolet light, as they reported this month in the American Chemical Society journal Nano Letters.
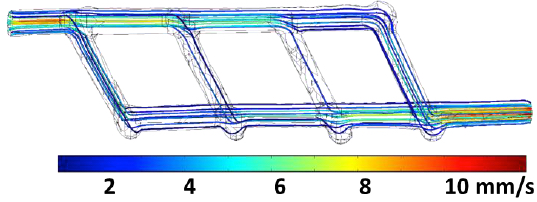
With each full revolution, the motor’s tail-like propeller moves the sub forward 18 nanometers, but with the motors running at more than a million RPM, that translates into almost 1 inch per second — a breakneck pace on the molecular scale, says Tour. “These are the fastest-moving molecules ever seen in solution,” he said.

This chemical schematic shows the design of single-molecule nanosubmersibles created at Rice University. The nanosub’s fluorescent pontoons are blue; the motor is red. (credit: Victor García-López/Rice University)
While they can’t be steered yet, the study proves molecular motors are powerful enough to drive the sub-10-nanometer subs through solutions of moving molecules of about the same size. “This is akin to a person walking across a basketball court with 1,000 people throwing basketballs at him,” Tour said.
In 2006, Tour’s lab introduced the world to nanocars, single-molecule cars with four wheels, axles, and independent suspensions that could be “driven” across a surface (see “Rice scientists attach motor to single-molecule car“).
Tour said many scientists have created microscopic machines with motors over the years, but most have either used or generated toxic chemicals. He said a motor that was conceived in 2009 by a group in the Netherlands proved suitable for Rice’s submersibles, which were produced in a 20-step chemical synthesis.
“These motors are well-known and used for different things,” said lead author and Rice graduate student Victor García-López. “But we were the first ones to propose they can be used to propel nanocars and now submersibles.”
Operate like a bacteria’s flagellum

A nanosubmarine found in nature: this whip-like flagellum powers a bacterium’s swimming (credit: LadyofHats/CC)
The motors, which operate more like a bacteria’s flagellum than a propeller, complete each revolution in four steps. When excited by light, the double bond that holds the rotor to the body becomes a single bond, allowing it to rotate a quarter step. As the motor seeks to return to a lower energy state, it jumps adjacent atoms for another quarter turn. The process repeats as long as the light is on.
For comparison tests, the lab also made submersibles with no motors, slow motors, and motors that paddle back and forth. All versions of the submersibles have pontoons that fluoresce red when excited by a laser, according to the researchers.
Once built, the sub’s performance was independently confirmed by Gufeng Wang at North Carolina State University.
Rice’s researchers hope future nanosubs will be able to carry cargoes for medical and other purposes. “There’s a path forward,” García-López said. “This is the first step, and we’ve proven the concept. Now we need to explore opportunities and potential applications.”
Wang is an assistant professor of analytical chemistry at North Carolina State. Tour is the T.T. and W.F. Chao Chair in Chemistry as well as a professor of computer science and of materials science and nanoengineering.
The National Science Foundation, the National Institutes of Health, the Welch Foundation, and North Carolina State supported the research.
Abstract of Unimolecular Submersible Nanomachines. Synthesis, Actuation, and Monitoring
Unimolecular submersible nanomachines (USNs) bearing light-driven motors and fluorophores are synthesized. NMR experiments demonstrate that the rotation of the motor is not quenched by the fluorophore and that the motor behaves in the same manner as the corresponding motor without attached fluorophores. No photo or thermal decomposition is observed. Through careful design of control molecules with no motor and with a slow motor, we found using single molecule fluorescence correlation spectroscopy that only the molecules with fast rotating speed (MHz range) show an enhancement in diffusion by 26% when the motor is fully activated by UV light. This suggests that the USN molecules give ∼9 nm steps upon each motor actuation. A non-unidirectional rotating motor also results in a smaller, 10%, increase in diffusion. This study gives new insight into the light actuation of motorized molecules in solution.