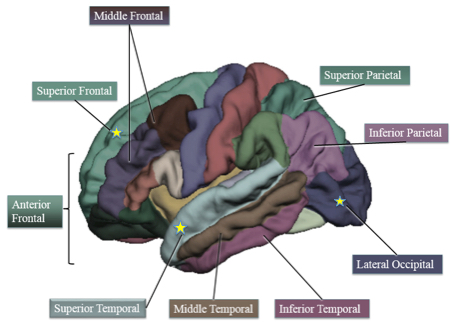
Life expectancy at birth, both sexes, 2013 (credit: Institute for Health Metrics and Evaluation)
The good news: as for 2013, global life expectancy for people in 188 countries has risen 6.2 years since 1990 (65.3 to 71.5). The bad news: healthy life expectancy (HALE) at birth rose by only 5.4 years (56.9 to 62.3), due to fatal and nonfatal ailments (interactive visualization by country here).
In other words, people are living more years with illness and disability. Ischemic heart disease, lower respiratory infections, and stroke cause the most health loss around the world.
That’s according to a study published in the medical journal The Lancet on August 27, conducted by an international consortium of researchers working on the Global Burden of Disease study, led by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington.
“The world has made great progress in health, but now the challenge is to invest in finding more effective ways of preventing or treating the major causes of illness and disability,” said Professor Theo Vos of IHME, the study’s lead author.
For dozens of countries — including Botswana, Belize, and Syria — healthy life expectancy in 2013 was not significantly higher than in 1990. In some of those countries, including South Africa, Paraguay, and Belarus, healthy life expectancy has actually dropped (by as much as 10 years) since 1990.
Causes of health loss
The fastest-growing global cause of health loss between 1990 and 2013 was HIV/AIDS, which increased by 341.5%. But this dramatic rise masks progress in recent years; since 2005, health loss due to HIV/AIDS has diminished by 23.9% because of global focus on the disease. Ischemic heart disease, stroke, low back and neck pain, road injuries, and COPD have also caused an increasing amount of health loss since 1990.The impact of other ailments, such as diarrheal diseases, neonatal preterm birth complications, and lower respiratory infections, has significantly declined.
Across countries, patterns of health loss vary widely. The countries with the highest rates of DALYs are among the poorest in the world, and include several in sub-Saharan Africa: Lesotho, Swaziland, Central African Republic, Guinea-Bissau, and Zimbabwe. Countries with the lowest rates of health loss include Italy, Spain, Norway, Switzerland, and Israel.
The number of DALYs due to communicable, maternal, neonatal, and nutritional disorders has declined steadily, from 1.19 billion in 1990 to 769.3 million in 2013, while DALYs from non-communicable diseases have increased steadily, rising from 1.08 billion to 1.43 billion over the same period.
Ethiopia: a case study in progress
Ethiopia is one of several countries that have been rising to the challenge to ensure that people live lives that are both longer and healthier. In 1990, Ethiopians could expect to live 40.8 healthy years. But by 2013, the country saw an increase in healthy life expectancy of 13.5 years — more than double the global average — to 54.3 years.
“Ethiopia has made impressive gains in health over the past two decades, with significant decreases in rates of diarrheal disease, lower respiratory infection, and neonatal disorders,” said Dr. Tariku Jibat Beyene of Addis Ababa University. “But ailments such as heart disease, COPD, and stroke are causing an increasing amount of health loss. We must remain vigilant in addressing this new reality of Ethiopian health.”
Countries with highest healthy life expectancy, both sexes, 2013
1 Japan
2 Singapore
3 Andorra
4 Iceland
5 Cyprus
6 Israel
7 France
8 Italy
9 South Korea
10 Canada
Countries with lowest healthy life expectancy, both sexes, 2013
1 Lesotho
2 Swaziland
3 Central African Republic
4 Guinea-Bissau
5 Zimbabwe
6 Mozambique
7 Afghanistan
8 Chad
9 South Sudan
10 Zambia
Leading causes of DALYs or health loss globally for both sexes, 2013
1 Ischemic heart disease
2 Lower respiratory infection
3 Stroke
4 Low back and neck pain
5 Road injuries
6 Diarrheal diseases
7 Chronic obstructive pulmonary disease
8 Neonatal preterm birth complications
9 HIV/AIDS
10 Malaria
Abstract of Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition
Background: The Global Burden of Disease Study 2013 (GBD 2013) aims to bring together all available epidemiological data using a coherent measurement framework, standardised estimation methods, and transparent data sources to enable comparisons of health loss over time and across causes, age–sex groups, and countries. The GBD can be used to generate summary measures such as disability-adjusted life-years (DALYs) and healthy life expectancy (HALE) that make possible comparative assessments of broad epidemiological patterns across countries and time. These summary measures can also be used to quantify the component of variation in epidemiology that is related to sociodemographic development.
Methods: We used the published GBD 2013 data for age-specific mortality, years of life lost due to premature mortality (YLLs), and years lived with disability (YLDs) to calculate DALYs and HALE for 1990, 1995, 2000, 2005, 2010, and 2013 for 188 countries. We calculated HALE using the Sullivan method; 95% uncertainty intervals (UIs) represent uncertainty in age-specific death rates and YLDs per person for each country, age, sex, and year. We estimated DALYs for 306 causes for each country as the sum of YLLs and YLDs; 95% UIs represent uncertainty in YLL and YLD rates. We quantified patterns of the epidemiological transition with a composite indicator of sociodemographic status, which we constructed from income per person, average years of schooling after age 15 years, and the total fertility rate and mean age of the population. We applied hierarchical regression to DALY rates by cause across countries to decompose variance related to the sociodemographic status variable, country, and time.
Findings: Worldwide, from 1990 to 2013, life expectancy at birth rose by 6·2 years (95% UI 5·6–6·6), from 65·3 years (65·0–65·6) in 1990 to 71·5 years (71·0–71·9) in 2013, HALE at birth rose by 5·4 years (4·9–5·8), from 56·9 years (54·5–59·1) to 62·3 years (59·7–64·8), total DALYs fell by 3·6% (0·3–7·4), and age-standardised DALY rates per 100 000 people fell by 26·7% (24·6–29·1). For communicable, maternal, neonatal, and nutritional disorders, global DALY numbers, crude rates, and age-standardised rates have all declined between 1990 and 2013, whereas for non–communicable diseases, global DALYs have been increasing, DALY rates have remained nearly constant, and age-standardised DALY rates declined during the same period. From 2005 to 2013, the number of DALYs increased for most specific non-communicable diseases, including cardiovascular diseases and neoplasms, in addition to dengue, food-borne trematodes, and leishmaniasis; DALYs decreased for nearly all other causes. By 2013, the five leading causes of DALYs were ischaemic heart disease, lower respiratory infections, cerebrovascular disease, low back and neck pain, and road injuries. Sociodemographic status explained more than 50% of the variance between countries and over time for diarrhoea, lower respiratory infections, and other common infectious diseases; maternal disorders; neonatal disorders; nutritional deficiencies; other communicable, maternal, neonatal, and nutritional diseases; musculoskeletal disorders; and other non-communicable diseases. However, sociodemographic status explained less than 10% of the variance in DALY rates for cardiovascular diseases; chronic respiratory diseases; cirrhosis; diabetes, urogenital, blood, and endocrine diseases; unintentional injuries; and self-harm and interpersonal violence. Predictably, increased sociodemographic status was associated with a shift in burden from YLLs to YLDs, driven by declines in YLLs and increases in YLDs from musculoskeletal disorders, neurological disorders, and mental and substance use disorders. In most country-specific estimates, the increase in life expectancy was greater than that in HALE. Leading causes of DALYs are highly variable across countries.
Interpretation: Global health is improving. Population growth and ageing have driven up numbers of DALYs, but crude rates have remained relatively constant, showing that progress in health does not mean fewer demands on health systems. The notion of an epidemiological transition—in which increasing sociodemographic status brings structured change in disease burden—is useful, but there is tremendous variation in burden of disease that is not associated with sociodemographic status. This further underscores the need for country-specific assessments of DALYs and HALE to appropriately inform health policy decisions and attendant actions.
Funding: Bill & Melinda Gates Foundation.