(credit: iStock)
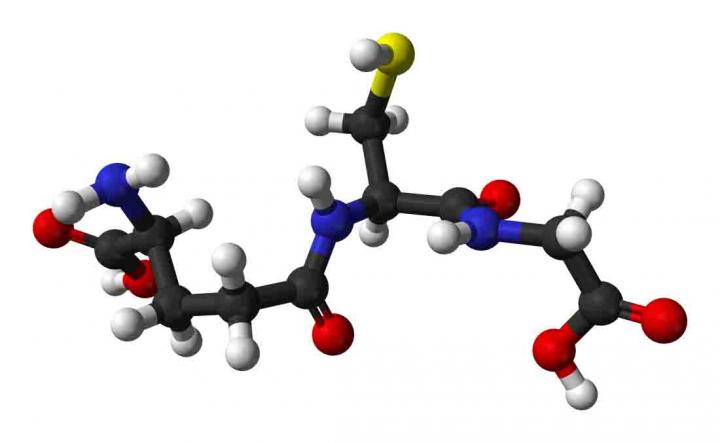
In the first controlled clinical trial of nicotinamide riboside (NR), a newly discovered form of Vitamin B3, researchers have shown that the compound is safe for humans and increases levels of a cell metabolite called NAD+ that is critical for cellular energy production and protection against stress and DNA damage.
Levels of NAD+ (first discovered by biochemists in 1906) diminish with age, and it has been suggested that loss of this metabolite may play a role in age-related health decline.
Studies in mice previously showed that boosting the levels of NAD+ can produce multiple health benefits, including resistance to weight gain, improved control of blood sugar and cholesterol, reduced nerve damage, and longer lifespan.* These findings have spurred people to take commercially available NR supplements designed to boost NAD+. However, these over-the-counter supplements have not undergone clinical trials to see if they work in people.
Human clinical trial shows NR is safe, boosts human NAD+ metabolism
The new research, reported Oct. 10 in the open-access journal Nature Communications, determined the time and dose-dependent effects of NR on blood NAD+ metabolism in humans. It was led by Charles Brenner, PhD, professor and Roy J. Carver Chair of Biochemistry at the University of Iowa Carver College of Medicine in collaboration with colleagues at Queens University Belfast and ChromaDex Corp., which supplied the NR used in the trial.**
The human trial involved six men and six women, all healthy. Each participant received single oral doses of 100 mg, 300 mg, or 1,000 mg of NR in a different sequence with a seven-day gap between doses. After each dose, blood and urine samples were collected and analyzed by Brenner’s lab to measure various NAD+ metabolites in a process called metabolomics.
The trial showed that the NR vitamin increased NAD+ metabolism by amounts directly related to the dose, and there were no serious side effects with any of the doses.
“This trial shows that oral NR safely boosts human NAD+ metabolism,” Brenner says. “We are excited because everything we are learning from animal systems indicates that the effectiveness of NR depends on preserving and/or boosting NAD+ and related compounds in the face of metabolic stresses. Because the levels of supplementation in mice that produce beneficial effects are achievable in people, it appears than health benefits of NR will be translatable to humans safely.”
The next step will be to study the effect of longer duration NR supplementation on NAD+ metabolism in healthy adults, but Brenner also has plans to test the effects of NR in people with diseases and health conditions, including elevated cholesterol, obesity and diabetes, and people at risk for chemotherapeutic peripheral neuropathy.
In addition to Brenner, the research team included researchers at the UI Carver College of Medicine, Queens University Belfast, and ChromaDex.
The research was funded in part by grants from the National Institutes of Health, the Biotechnology and Biological Sciences Research Council, the Roy J. Carver Trust, and ChromaDex.
** The mouse study showed that NAAD is formed from NR and confirmed that NAAD levels are a strong biomarker for increased NAD+ metabolism. The experiments also revealed more detail about NAD+ metabolic pathways.
In particular, the researchers compared the ability of all three NAD+ precursor vitamins — NR, niacin, and nicotinamide — to boost NAD+ metabolism and stimulate the activity of certain enzymes, which have been linked to longevity and health benefits. The study showed for the first time that oral NR is superior to nicotinamide, which is better than niacin in terms of the total amount of NAD+ produced at an equivalent dose. NR was also the best of the three in stimulating the activity of sirtuin enzymes. However, in this case, NR was the best at stimulating sirtuin-like activities, followed by niacin, followed by nicotinamide.
The information from the mouse study subsequently helped Brenner’s team design the formal clinical trial. In addition to showing that NR boosts NAD+ in humans without adverse effects, the trial confirmed that NAAD is a highly sensitive biomarker of NAD+ supplementation in people.
** Brenner is a consultant for ChromaDex. He also is co-founder and Chief Scientific Adviser of ProHealthspan, which sells NR supplements under the trade name Tru NIAGEN. Prior to the formal clinical trial, Brenner conducted a pilot human study — on himself. In 2004, he had discovered that NR is a natural product found in milk and that there is pathway to convert NR to NAD+ in people. More than a decade of research on NR metabolic pathways and health effects in mice and rats had convinced him that NR supplementation had real promise to improve human health and wellness.
After consulting with UI’s institutional review board, he conducted an experiment in which he took 1 gram of NR once a day for seven days, and his team analyzed blood and urine samples using mass spectrometry. The experiment showed that Brenner’s blood NAD+ increased by about 2.7 times. In addition, though he reported immediate sensitivity to flushing with the related compound niacin, he did not experience any side effects taking NR.
The biggest surprise from his metabolomic analysis was an increase in a metabolite called NAAD, which was multiplied by 45 times, from trace levels to amounts in the micromolar range that were easily detectable.
“While this was unexpected, I thought it might be useful,” Brenner says. “NAD+ is an abundant metabolite and it is sometimes hard to see the needle move on levels of abundant metabolites. But when you can look at a low-abundance metabolite that goes from undetectable to easily detectable, there is a great signal to noise ratio, meaning that NAAD levels could be a useful biomarker for tracking increases in NAD+ in human trials.”
Brenner notes this was a case of bidirectional translational science; having learned something from the initial human experiment, his team was able to return to laboratory mice to explore the unexpected NAAD finding in more detail.
Abstract of Nicotinamide riboside is uniquely and orally bioavailable in mice and humans
Nicotinamide riboside (NR) is in wide use as an NAD+ precursor vitamin. Here we determine the time and dose-dependent effects of NR on blood NAD+ metabolism in humans. We report that human blood NAD+ can rise as much as 2.7-fold with a single oral dose of NR in a pilot study of one individual, and that oral NR elevates mouse hepatic NAD+ with distinct and superior pharmacokinetics to those of nicotinic acid and nicotinamide. We further show that single doses of 100, 300 and 1,000 mg of NR produce dose-dependent increases in the blood NAD+ metabolome in the first clinical trial of NR pharmacokinetics in humans. We also report that nicotinic acid adenine dinucleotide (NAAD), which was not thought to be en route for the conversion of NR to NAD+, is formed from NR and discover that the rise in NAAD is a highly sensitive biomarker of effective NAD+ repletion.